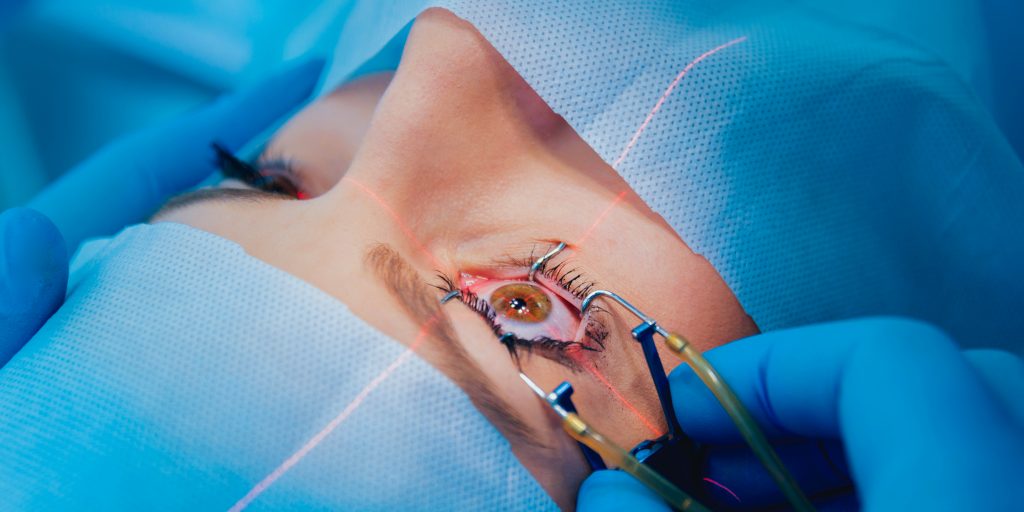
Laser Surgeries
The described techniques have been approved by many objective and Scientific Societies; the text used is recommended by the B.S.C.R.S (Belgian Society of Cataract & Refractive Surgery) in its brochures on Refractive Surgery, a common work of a panel of Ophthalmologists. The B.S.C.R.S. has 220 members, all Ophthalmologists.

Lasik and PRK techniques
These two techniques are the most frequently performed in refractive surgery. Refractive surgery means surgery of a refractive error, namely myopia, hyperopia and / or astigmatism. These two techniques require a sophisticated, technically advanced device, the excimer laser. This excimer laser removes tissue in the central part of the cornea (nearsighted people) and on the edge (far-sighted people). The areas where tissue is removed may be mixed for the correction of astigmatism.
The modern excimer lasers are equipped with a guiding system, which ensures a perfect centering of the treatment; this system follows the slightest movement of the eye during the operation even if the patient has difficulty fixing the aiming point. In addition, a special extremely accurate iris recognition system ensures a perfect alignment between the pre-operatively examinated eye with corneal topography and aberometry and the operated eye.
PRK
The ablation happens on the surface of the cornea; the surgeon has to remove the epithelium; this takes one minute, and then the laser can treat on this “new surface”. The treatment is short, less than one minute, and is not painful. At the end, the eye will be protected by a bandage contact lens, or by a patch.
Two variants of this technique: Epi-lasik (where the epithelium is removed with a special instrument, and Lasek, where the epithelium is removed with an alcohol solution.
Lasik
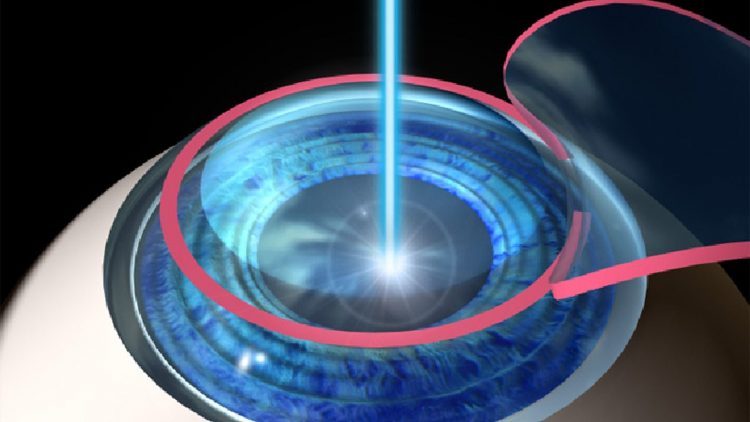
Here the ablation does not happen on the surface of the cornea, but in the cornea itself. The first step is to realize a flap, with a special instrument, called microkeratome, and to “open” this flap, exactly like when opening the hood of a car. The second step is to ablate with the laser on the corneal bed. After the ablation, the corneal flap is repositioned and the interface is rinsed. The flap adheres by itself, so a few minutes are needed to be sure that the flap is well in place. The patient is checked 30 minutes after the surgery to be sure that the flap adheres nicely on the eye before he leaves the center. A protective eye-shield is worn day and night for 3 days, and at night for one week. The treatment is not painful.
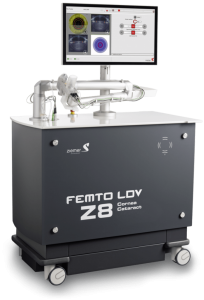
It is also possible to use another laser, called Femtosecond laser, to create the flap, instead of the microkeratome. This relatively new instrument can be interesting for some patients, althrough no study showed a better visual reabilitation with one instrument than with the other.
Indications for laser corrective surgery or refractive surgery
Patients with a myopia less than 10D, stable, over 18 years old, can consider the surgery as an alternative to glasses or contact lenses; patients wishing to have a “normal” life without optical devices can also consider refractive surgery; sportsmen and some professionals where there is a requirement for good functional vision without glasses could be candidates. Finally, people unable to wear lenses for different reasons, could be helped by this surgery.
Hyperopia up to 4D can be corrected; but over 4D, there is most of the time a partial correction, which already helps, but does not solve the problem completely.
Astigmatism (combined with myopia, hyperopia, or pure astigmatism) can also be addressed by today’s lasers up to 6D.
It is generally admitted that Lasik will give best results for myopia over 5 or 6D, with a faster recovery and less pain than PRK, more indicated for lower correction. However, some patients, despite their refractive error, will be poor candidates for one particular technique and will be counselled for another technique, or not to have refractive surgery (large pupils, unstable refraction, thin corneas, unpredictable results, unrealistic visual expectations,…).
It is obvious that the surgery will never happen without a careful eye examination, conducted by the surgeon himself and his co-workers. This ensures that the surgery can be done with the best chances of success. The technique is fully explained to the candidate, and a brochure is given at all times, to be sure that he/she has enough understanding of the procedure.
Risks of corneal refractive surgery
The first risk of any surgery is always infection. To avoid this, antibiotics eye drops are given; the patient must be prudent for a couple of days, should not rub his/her eyes, must keep the contact lens, or the patch, or the eye-shield depending on the technique.
It is forbidden to swim for at least 2 weeks; no make-up should be used for the same period. The eyes can be relatively dry after the surgery, so artificial tears must be used frequently.
There is always a possibility to experience some pain, especially after PRK for a couple of days; painkillers in tablets or in drops will help.
Some risks are linked to the technique used:
- for PRK: delay in visual recovery because healing is slower; haze (a kind of mist) formation in the cornea, slowly disappearing with time; light sensitivity, etc…
- for Lasik: the flap creation is crucial: the flap must have the right thickness, the right diameter, and the right size. If for any reason, the flap is not perfect, the laser ablation will not be done, but a new attempt can be realized a few months later. After the surgery, some flaps might present little folds, impairing vision and slowly disappearing with time. Dryness, light sensitivity, can also result in vision difficulties.
This is a short list of possible complications. However, it should be kept in mind that the risk of having a sight threatening complication is low; your surgeon will help you by advising you the best technique in your case and the results you can expect. The risks in your case will also be explained.
It is generally admitted in scientific meetings that +/- 85 to 95% of the cases, depending on their preop refractive error will be able to function without optical devices, and that 5 to 15% of the cases will need them for special circumstances (night driving, TV, …).
Reimbursement and special
In Belgium, the I.N.A.M.I. will not reimburse refractive surgery; however, some private insurances will, depending on the contract one particular individual might have subscribed.
Some professions where a full medical examination is required, might have special criteria regarding refractive surgery; it is therefore necessary that the candidate fully understands the requirements relative to his/her job.
It must be understood that the few explanations given above will never replace the advice of a specialized surgeon in refractive surgery. They are only here to help you to better understand the techniques and their different aspects. However, full explanations are a must and are given during the consultation, after a documented eye exam.
Certaines professions, dont l’accès peut être soumis à un examen médical complet, peuvent avoir des critères particuliers concernant la chirurgie réfractive; il appartient donc au futur candidat de se renseigner de manière approfondie avant toute opération et d’avoir parfaitement compris les critères d’acuité visuelle requis pour l’exercice de la profession exercée ou envisagée.
Enfin, il faut réaliser que toutes les explications reprises ci-dessus ne remplaceront jamais les conseils d’un chirurgien expérimenté en chirurgie réfractive. Ces quelques lignes ont pour but essentiel de vous aider à comprendre les techniques utilisées et leurs différents aspects. Les explications plus détaillées et personnalisées sont toujours données lors de la consultation, après un examen ophtalmologique approfondi.
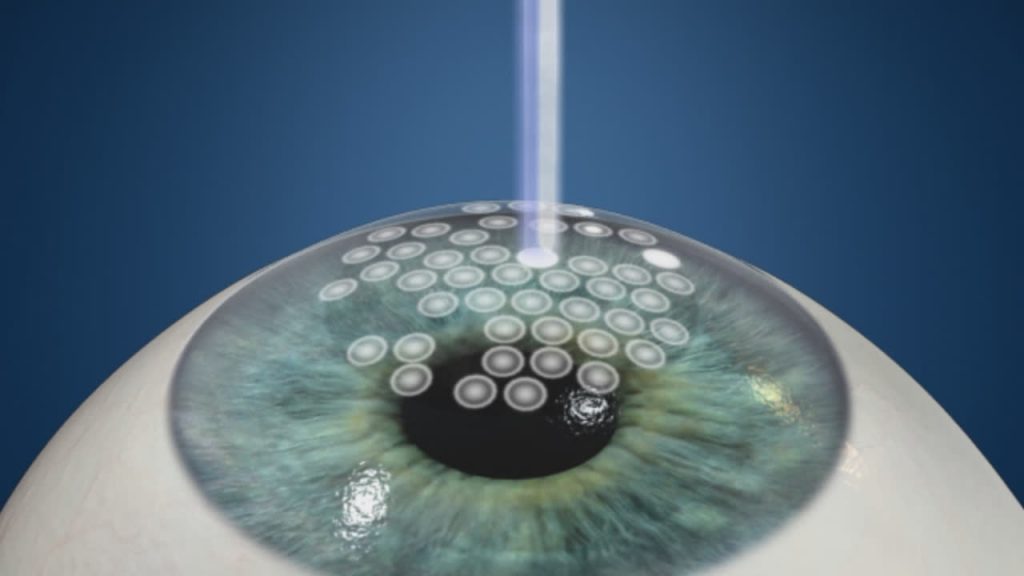
Customized ablations and wavefront analysis.
This is a progress in refractive surgery and seems to become the future. If you are myope of -3 Diopters, you will receive the same glasses, or lenses, or refractive laser procedure as any myope of -3 Diopters.
And yet, you are not the same person, and your right eye is probably not the same as your left eye, while the defect seems the same on both sides. From this was born the idea of a personalized, tailor-made treatment, adapted to each case, therefore to each patient, but also to each eye and to the aberrations of the eye. What is aberration? If a “bright” ray is emitted and projected into the eye, it will be sent back – reflected – and can be analyzed by the computer. Its characteristics are unique and its modifications or alterations will be called “aberrations”.
Some people have more aberrations than others.
It is therefore interesting to know before the treatment who will benefit most from a personalized treatment, because most studies show that only patients with high-order aberrations will actually benefit from this technique.
The goal is not only to improve visual acuity, but also to improve the quality of vision, for example, in the evening, low contrast, night driving, etc.
Studies show that +/- 18% of patients have better vision in poor light than before surgery; an even higher percentage of cases have fewer halo and glare complaints.
DO YOU HAVE ANY QUESTIONS?
We will be happy to answer you as soon as possible.